What happens when your nearest major hospital is over an hour’s drive away?
According to these residents of Berwick Upon Tweed, it means feeling “a million miles from help”.
As plans for Berwick’s new infirmary are discussed, a group of campaigners in the North Northumberland town are arguing “the NHS needs to do more” for the people of the area.
What began as a group of locals concerned about the scheme to combine the sites of a new hospital and leisure centre has become something with a far broader remit.
Fighting for “a better hospital for Berwick”, campaigners argue the area has been left behind, seeing a gradual reduction in services over 30 years. They say the plans, which will maintain the services currently offered, with a reduction in beds from 20 to 16, leave the town without enough health services.

They say journeys to and from Wansbeck and Cramlington hospitals - 50 and 60 miles away respectively - sometimes for very short appointments, are taking their toll, while many are afraid of any medical emergency, knowing that any ambulance journey means an hour spent on the A1 before doctors can even see them.
Northumbria Healthcare NHS Foundation Trust say it wouldn’t be possible to bring services like Accident and Emergency to Berwick, as they couldn’t operate safely.
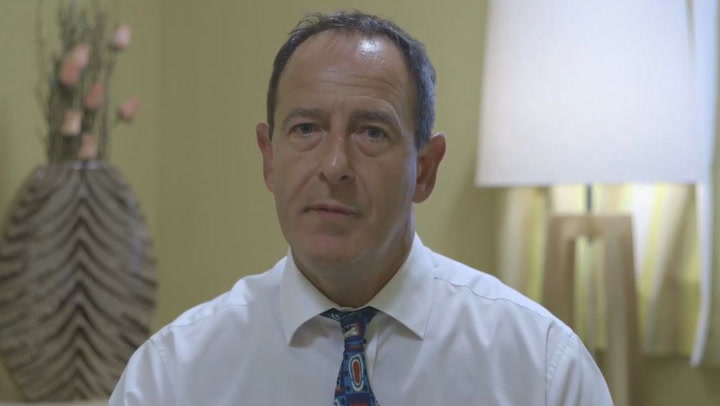
Medical director Dr Colin Doig said: “We are committed to providing services closer to home when it is safe and sustainable to do so to save people travelling out of the area.
“Thousands of local people receive care at Berwick Infirmary every year and this will continue to happen in the new hospital which represents a £25 million investment in healthcare. The new hospital will deliver all the existing services and offer an exciting opportunity to provide care in a much-improved, modern setting.

“In today’s NHS, specialist services cannot be provided in every local hospital due to the level of expertise and sophisticated equipment required. These services must be delivered across a large population to enable specialist teams to treat the right volume of patients to maintain their skills.
“We would urge anyone who has difficulty travelling to access an appointment at one of our hospitals to get in touch with us on 01289 356625.”
The trust also says it expects to see an increase in “virtual clinics” enabling people to see specialists in other hospitals at a distance.
But Berwick residents say their town needs more.
Here are four people who say their lives have been blighted by hours upon hours of travelling to access healthcare:
Wade

Simon Garland’s son 10-month-old Wade “had a lot of hardship coming into this world”, spending the first three weeks of his life in intensive care at the RVI. Simon says it was in December, when Wade began struggling to breathe, that he realised his local hospital didn’t have the equipment needed to help with the feeding tube Wade uses.
Simon said: “The staff have been spectacular in trying their hardest to look after Wade and his needs but due to the lack of facilities in Berwick they are unable to help us.
“We were trained in the RVI on how to put in Wade’s feeding tube, as we were told that Berwick can’t do and if we did not learn we would have to travel to Cramlington if he pulled it out, so after the district nurses had finished for the day we were totally on our own with an ill baby 60 miles from the hospital that can help.
“This made us feel so alone and unsupported - a million miles from help would best describe the feeling.”
Wade, who suffers from brain damage, issues with reflux, and has a preliminary diagnosis of cerebral palsy, has to visit specialists in the RVI and at Wansbeck, which can mean the whole family has to take a full day off work for a half hour appointment because travelling with him is so difficult. But it’s being so far from emergency help that fills the family with fear.
“I’ve lived in Berwick my whole life, Berwick is my home, but it makes us seriously consider upping our family and moving,” his dad said.
Zachariah

Edward Frank’s son Zachariah has just turned two - but he’s already made seven emergency ambulance trips in his short life. Zachariah suffers from breathing problems, which sometimes mean he needs specialist care - but sometimes need more simple treatments, like doses of steroids. Edward says on one occasion his family was taken to the Borders General Hospital, over 30 miles away in Scotland, because out of hours there was no one at Berwick able to prescribe the steroids he needed. On other occasions, Edward suffers from seizures, while his wife Shirley is registered blind, so neither can drive. This means they’ve been forced to stay in hospitals miles from home waiting for transport back after emergency visits, while routine appointments can mean round trips of over three hours for the young family.
Edward said: “I don’t think we can expect Berwick to have a sick children’s unit or all the bells and whistles, but we’ve lost a lot over the last 30 years. Zachariah will need to visit specialists all his life, and I understand that, but there could be more common, emergency services here. It could put people’s lives at risk if they have to wait.
“I can’t fault the staff at Berwick or the ambulance crews, but more needs to be done by the NHS to help the people of Berwick.”
Joan

Joan Arnfield, 79, suffered from macular degeneration and peripheral vascular disease.
She has to visit Cramlington Hospital every four to six weeks for injections in her eyes, or risk losing her sight completely. She uses hospital transport, which she says she “appreciate[s] very much” but the long journey, which she has been doing for six years, has become something she “dreads”.
Joan said: “There are times i don’t want to do the 120m round trip as I feel too unwell, but if I stop going for the treatment I will surely lose my sight.
“I do appreciate the transport to get me there, but it’s a dread.”
Kathryn

Kristine Reilly’s 18-year-old daughter Kathryn suffers from asthma so severe it can be life threatening.
Her condition is so serious she has to receive specialist treatment at the RVI, meaning Kristine says she’s spent tens of thousands of pounds in fuel travelling up and down the A1 in the six years since she moved to Berwick. She says the hospital doesn’t have the capacity to check her daughter’s lung function, so whenever the family have worries, they must face journeys of over an hour.
She said: “Kathryn does need specialist care and I understand that, if we have to go to the RVI we have to go, but I would feel so much better if she could have her lung function tested at Berwick. She doesn’t need specialist care every time.
“The constant journeys have the most traumatic effect, the anxiety I feel whenever I have to go down that road is indescribable.
Kristine claims the distance between Berwick and emergency services has a huge psychological impact, not just on her family, but on much of the town.
“This community is scared to get sick,” she said.